ANAL FISSURE
What is an anal fissure?
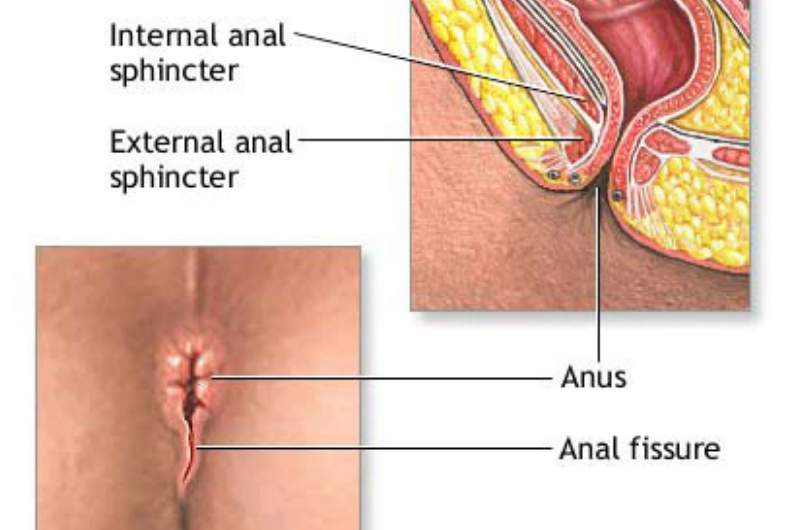
An anal fissure is a tear in the lining of the lower rectum (anal canal) that causes pain during bowel
movements. Anal fissures don’t lead to more serious problems.
Most anal fissures heal with home treatment after a few days or weeks. These are called short-term (acute)
anal fissures. If you have an anal fissure that hasn’t healed after 8 to 12 weeks, it is considered a
long-term (chronic) fissure. A chronic fissure may need medical treatment.
Anal fissures are a common problem. They affect people of all ages, especially young and otherwise healthy
people.
WHAT CAUSES AN ANAL FISSURE?
Anal fissures are caused by injury or trauma to the anal canal. Injury can happen when:
- You pass a large stool.
- You are constipated and try to pass a hard stool.
- You have repeated diarrhea.
- You give birth. (Childbirth can cause trauma to the anal canal.) Fissures can also be caused by a rectal exam, anal intercourse, or a foreign object. In some cases, a fissure may be caused by Crohn’s disease.
- Many experts believe that extra tension in the two muscular rings (sphincters) controlling the anus may be a cause of fissures. The outer anal sphincter is under your conscious control. But the inner sphincter is not. This muscle is under pressure, or tension, all of the time. If the pressure increases too much, it can cause spasm and reduce blood flow to the anus, leading to a fissure. This pressure can also keep a fissure from healing.
WHAT ARE THE SYMPTOMS?
You may have:
- A sharp, stinging, or burning pain during bowel movements. Pain from a fissure may be quite severe. It can be brief or last for several hours after a bowel movement.
- Bleeding. You may see a small spot of bright red blood on toilet tissue or a few drops in the toilet bowl. The blood from a fissure is separate from the stool. (Very dark, tarry stools or dark red blood mixed with stool may be a sign of a more serious problem.) Tell your doctor if you have any bleeding with a bowel movement.
- Sometimes an anal fissure may be a painless wound that won’t heal. It may bleed from time to time but cause no other symptoms.
HOW IS AN ANAL FISSURE DIAGNOSED?
A doctor can diagnose an anal fissure based on your symptoms and a physical exam. The exam may include:
- Looking at the fissure by gently separating the buttocks.
- A digital rectal exam. The doctor inserts a gloved finger into the anal canal.
- Anoscopy. This involves using a short, lighted scope to look into the anal canal. The doctor may wait until the fissure has started to heal before doing a rectal exam or anoscopy. If an exam needs to be done right away, medicine can be used to numb the area.
During an exam, a doctor can also find out whether another condition may be causing the fissure. Having several fissures or having one or more in an area of the anus where fissures usually don’t occur can be a sign of a more serious problem, such as inflammatory bowel disease or a weakened immune system.
MEDICATIONS
Topical anaesthetics
A topical medicine is one that you apply directly to the affected area. Topical anaesthetics work by desensitising (numbing) the skin, which in the case of an anal fissure, will help ease the sharp and severe pain you may experience when passing stools.
Lidocaine is the most commonly prescribed topical anaesthetic. It either comes in the form of a gel or an ointment. Lidocaine is usually only used for one to two weeks because the fissure should start to heal within this time. It is usually applied shortly before passing a stool, but you should always follow the instructions that come with the medicine.
Painkillers
If you experience prolonged, burning pain after passing stools, you may be prescribed an analgesic (painkiller) such as paracetamol or ibuprofen. Again, you should always follow the dosage instructions on the patient information leaflet or packet.
FOLLOW-UP
Your GP will usually arrange for you to have a follow-up appointment, approximately eight weeks after the start of your treatment. This will enable them to check that your fissure has healed, or is showing adequate signs of improvement. If your condition has not been completely treated, your GP may recommend a further follow-up appointment six to eight weeks later.
If your anal fissure is particularly severe, or does not respond to treatment after eight weeks, you may have to be referred to a proctologist (a doctor who specialises in conditions that affect the rectum and anus) for specialist treatment. This will usually involve having some type of surgery.
SURGERY
There are a number of different surgical techniques that can be used to treat an anal fissure. These are
discussed
below. Internal sphincterotomy
An internal sphincterotomy involves removing a section of the sphincter muscle. This helps to reduce the
tension in the
muscle, preventing further spasms of the sphincter and allowing the anal fissure to heal.
An internal sphincterotomy is a relatively straightforward operation that can be performed using a local
anaesthetic on
a day patient basis, which means you will not have to spend the night in hospital.
An internal sphincterotomy is an effective treatment with a good track record of success. Around 95% of
people who have
this type of surgery will experience healing of their anal fissure.
Around 1 in 10 people will experience bowel incontinence after having surgery due to damage to the anal
muscles. This
means they will lose some control of their bowel movements. However, it is usually a mild type of
incontinence where the
person is unable to prevent themselves from passing wind, and they may also experience some mild soiling.
The symptoms of incontinence usually improve in the first few months after surgery and resolve within two
months.
However, in around 1 in 200 cases the incontinence is permanent.
Read more about bowel incontinence.
FISSURECTOMY
A fissurectomy is the surgical removal of an anal fissure, along with the surrounding tissue. Fissurectomies are not as widely used as internal sphincterotomies because they do not treat the underlying causes. Therefore, a fissurectomy may not prevent anal fissures from reoccurring in the future. However, a fissurectomy may be a recommended treatment option for children because removing a section of the sphincter muscle at an early age could cause permanent incontinence.
ADVANCEMENT ANAL FLAPS
Advancement anal flaps involve taking healthy tissue from another part of your body and using it to repair the fissure and improve the blood supply to the site of the fissure. This is often recommended to treat cases of chronic anal fissure, which have occurred as a result of pregnancy or other injury to the anus.
Make an Appointment