IDIOPATHIC ULCERATIVE COLITIS
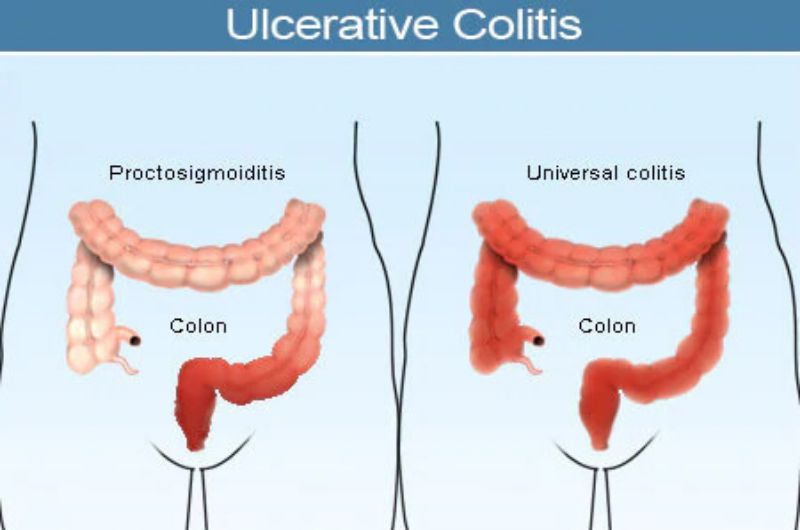
Ulcerative colitis (UC) is a type of inflammatory bowel disease (IBD) that affects the large intestine.
The large intestine consists of the cecum, ascending/tranverse/descending/sigmoid colon and
rectum. UC
usually begins in the rectum and may continue up into the colon. When inflamed, the intestinal
lining can
become red, swollen, develop ulcers and bleed. This inflammation and irritation can prevent the
large
intestine from absorbing enough fluid and salt from stool, leading to diarrhea.
UC is a chronic, lifelong disease with alternating periods of activity and remission. Patients
may
experience intense symptoms followed by varying periods of time when the symptoms seem to
disappear.
The cause of ulcerative colitis is unknown, but it appears to involve dysfunction of the immune
system.
Protective cells normally present in the gastrointestinal lining are triggered to attack when
bacteria and
viruses pass through the digestive tract. In patients with ulcerative colitis, this attack
continues, even
when harmful substances are no longer present – leading to chronic inflammation and irritation.
It is not
clear whether this immune dysfunction is a cause or result of UC.
UC appears most often in people between the ages of 15 and 35, but may also occur in older or
younger
populations. About 500,000 Americans have UC, according to the Crohn's & Colitis Foundation of
America
(CCFA). Another 500,000 have Crohn's disease (CD), the other major type of IBD.
Ulcerative colitis differs from Crohn's disease in a number of ways. In patients with ulcerative
colitis,
only the large intestine is affected whereas CD may occur anywhere throughout the digestive
tract, including
the small and large intestines. Inflammation caused by UC is usually continuous, without any
normal tissue
appearing between inflamed areas. In CD, there may be patches of normal tissue between inflamed
areas. In
addition, UC affects only the inner lining of the intestine, so ulcers are not likely to break
through the
innermost intestinal wall layer (mucosa), as may occur in patients with CD.
Inflammatory bowel diseases such as UC and Crohn's disease are sometimes confused with irritable
bowel
syndrome (IBS). However, IBS does not involve inflammation of the intestines, which is present
in both UC
and CD. Also, IBS does not include bloody diarrhea as a symptom and IBS tests reveal no
abnormalities. IBS
is not associated with either ulcerative colitis or Crohn's disease.
HOW IS IT DIAGNOSED?
The first step in diagnosing ulcerative colitis (UC) is a visit to a physician for a medical
history and
physical examination. Individuals will present with the following complaints: rectal bleeding,
having to
strain to produce stools (tenesmus), repeated bouts of diarrhea then constipation, rectal
urgency, abdominal
cramping, fever, malaise, nausea and vomiting, joint pains (arthralgias), and night sweats. If
individuals
have a severe bout of ulcerative colitis, they will present to the physician with fever, body
fluid loss
(dehydration), increased heart rate (tachycardia), and abdominal tenderness.
Patients may be asked about the extent and duration of their symptoms, any family history of
inflammatory
bowel disease (IBD), as well as their eating, drinking or smoking habits.
Blood tests and stool samples may also be required. Blood tests can identify low red blood cell
counts
(anemia) and high white blood cell counts (which may indicate inflammation or infection). A
stool sample
analysis (fecal test) can identify bleeding or infection of the large intestine.
Make an Appointment